Stroke is the collective name for a disease that severely disrupts the blood supply to the brain. The old-fashioned and popular names are stroke, haemorrhagic stroke, cerebral palsy or cerebral infarction. The symptoms and consequences may be similar in all cases. Stroke is always a permanent condition, i.e. functions can usually not be restored. In lucky and mild cases, symptoms resolve within 24 hours and the loss of function is temporary. In these cases, it is not called a stroke but a transient ischaemic attack (TIA).
Ischaemic stroke
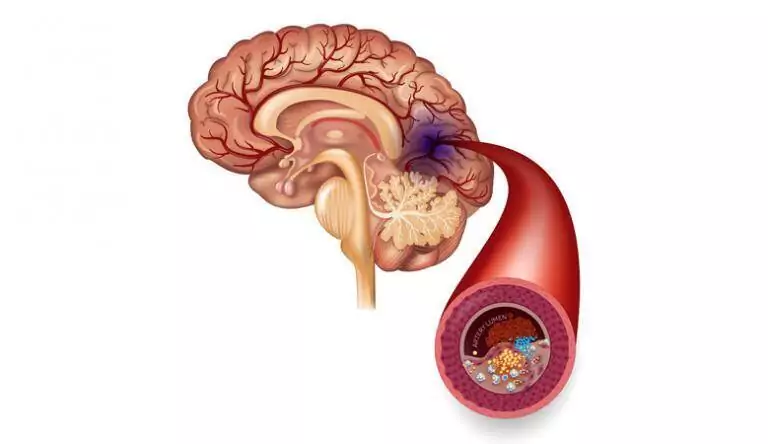
It occurs when the blood supply to an area of the brain is suddenly cut off, for example by a vasospasm, a vasoconstriction or an embolism (blood clot). The area of the brain without blood supply is deprived of oxygen and nerve cell function stops. If blood circulation is not restored within minutes, nerve cells (especially in the immediate vicinity of the blocked area) die. The functions provided by that brain area (e.g. speech, balance, movement, thinking, memory, perception, etc.) are lost. Ischemic stroke accounts for 70-80% of all cases.

Haemorrhagic stroke
Rarer than the ischaemic form. It occurs when a blood vessel within the skull “bursts”. It can be caused by a stiff vessel wall due to atherosclerosis, untreated high blood pressure (or a sudden spike in blood pressure due to skipping medication). In this scenario, the symptoms do not result from oxygen deprivation. A growing ‘pool of blood’ in the brain tissue or in the space between the layers of the meninges is suppressing the surrounding areas, causing dysfunction. As the space inside the skull is narrow, the bones do not ‘expand’, so the pressure tries to move towards the ‘old hole’ at the base of the skull. The increase in pressure presses against the bone, which is the breathing centre. If this stops working, it causes death.
Symptoms of stroke
- Sudden numbness or weakness (especially on one side of the body)
- Distraction
- Disturbance of speech or understanding
- Sudden loss of vision in one or both eyes
- Difficulty moving
- Dizziness, loss of balance or coordination
- Sudden, severe headache without known cause
Although stroke is a disease of the brain, the symptoms and consequences can severely affect the whole body.
- disturbance of cognition and thinking (cognitive functions)perception, focusing attention, counting and more complex thinking tasks (e.g. learning, decision-making, planning, problem-solving, self-awareness, etc.) become difficult or impossible. Memory problems, speech problems, emotional difficulties, daily living problems (self-care) and pain can make everyday life more difficult.
- paralysis (loss of muscle movement). Paralysis can affect only the face, but not the arm or leg. Hemiplegia is a more common form, affecting one side of the body, including the face, arm, and leg. The location of the paralysis can indicate which side of the brain is impacted. Paralysis on the left side is linked to issues in the right hemisphere, and conversely, right-sided paralysis is attributed to the left hemisphere.
Main risk factors for stroke
High blood pressure, heart disease, diabetes and smoking are the most important vascular damaging factors. An increase in the number of red blood cells, a heart rhythm disorder called atrial fibrillation, increases the risk of blood clot formation
Some doctors believe that 80% of strokes could be prevented. Reducing risk factors and consistently managing and controlling underlying conditions could help prevent stroke or significantly reduce the risk.
Treatment of stroke
If acute stroke symptoms are present, seek immediate emergency care. The time factor is important, i.e. you should get the patient to the hospital as soon as possible. The first few hours really matter for the outcome of the disease.
To treat an ischemic stroke, medical professionals remove the blockage and restore blood flow to the brain. In ischaemic stroke, there are fewer interventional options. If possible, the aim is to eliminate the source of the bleeding (e.g. an aneurysm).
When the blood supply to the brain is interrupted, the most affected brain cells die within a short time, while dysfunction predominates in the “peripheral zones”. The aim of treatment is to reduce or minimise the dead area.
Unfortunately, only a few percents of stroke patients arrive at a hospital with the right equipment in time. Unfortunately, it is a matter of minutes before permanent damage occurs.
In lucky cases, the brain can repair or mitigate the damage caused by a stroke. Brain cells that have not died may eventually regain function. Sometimes another region of the brain takes over some of the functions of the area damaged by the stroke. Some stroke survivors occasionally report unexplained, unexpected returns of function.
Treatment outcomes
- 10% of stroke survivors recover with almost no symptoms
- 25% are left with mild impairments that cause no or minimal difficulty in daily living
- 40% are left with impairments that require external help for certain tasks
- 10% become incapable of self-sufficiency, requiring long-term care by others
- 15% die shortly after a stroke
Rehabilitation
Once the intensive treatment has resolved the immediate threat to life and the general condition has stabilised, rehabilitation should begin immediately! Rehabilitation professionals should start treatment up to two days after a stroke. They should teach how to continue, what to practice and why, and how to improve after leaving hospital.
The aim of rehabilitation is to restore or at least improve the functions impaired by the stroke so that the survivor remains as independent as possible. The most difficult part is to motivate the patient, as unexpected and severe losses of ability can shock and depress the patient. They must be willing to relearn the basic skills that stroke has taken away – such as the ability to speak, eat, drink, dress and walk – because without them they become vulnerable to others.
There is also a lot of work for the family, as they often have to make home adaptations to adapt to the changed abilities after a stroke. Installing handrails, ramps, special utensils, cutlery, wheelchairs, patient lifts, etc. may be necessary. Implement material needs according to the individual condition, as they may vary for everyone.
Home medical technology in rehabilitation
Most people who suffer a stroke lose some ability to move. Some people just have weakened muscles because the nerve impulses are not getting to the muscles properly. Some have problems with motor coordination, for example, lifting a spoon into the mouth is almost impossible. Unused muscles quickly lose strength and mass (muscle atrophy), which we must prevent. In the case of a stroke, the affected muscles become spastic (stiff), making movement and coordination even more difficult.
Ergometers
Within a few days after a stroke, individuals can utilize home rehabilitation ergometers. More about the role of ergometers in stroke rehabilitation here.
[message title=”OxyCycle 3 active – passive ergometer” title_color=”#ffffff” title_bg=”#1e73be” title_icon=”” content_color=”#000000″ content_bg=”#ededed” id=””]
- Adjustable speed and resistance

- For both upper and lower limbs
- 15-minute timer switch
- Display showing elapsed time, RPM, total revolutions and calories burned
[/message]
Re-educating damaged nerves involves repeating the execution of movements. At first, the patient attempts unsuccessfully to raise the paralyzed hand. Because of the damage to the nerve-muscle connection, no movement is visible, so he does not know what he is supposed to do, or how to perform the movement correctly.
Biofeedback Stimulators – Assess and give feedback on movement rehabilitation
For these people, biofeedback devices are a fantastic help. Even when there is no muscle contraction, they detect the nerve impulse and transmit feedback indicating the initiation of the correct nerve “instruction.” For instance, the display will exhibit a diagram or emit a variable-intensity beep to signal whether the movement has been executed correctly. A higher value indicates better execution, meaning the patient knows exactly how the exercise was performed. The repetition, with feedback from the device, helps to restore the nerve-muscle connection and to perform the movement again with the correct strength and coordination.
[message title=”DuoBravo biofeedback/EMS – Rehabilitation after stroke” title_color=”#ffffff” title_bg=”#1e73be” title_icon=”” content_color=”#000000″ content_bg=”#ededed” id=””]
- Primary use in treatment of paralysis of central origin (e.g. after stroke)

- Regaining mobility lost due to stroke
- Relearning movement and preventing muscle atrophy and stiffness
- Biofeedback (EMG)
- ETS (biofeedback-induced stimulation)
[/message]
Biofeedback + muscle stimulator devices are even more effective. These not only provide feedback but when they detect the signal sent by the brain to the muscle. Furthermore, they actively deliver a muscle stimulation pulse to the treated muscle, inducing it to contract and assist in producing the desired movement. This dual reinforcement accelerates rehabilitation and additionally guarantees the maintenance and improvement of muscle strength. One such device is the DuoBravo biofeedback+EMS device.
In Summary
Technology – and medical technology is part of it – is advancing at an amazing pace! Today’s state-of-the-art machines provide a useful aid in treatment that was unimaginable even a few years ago! In the past, paralysis caused by stroke almost always led to permanent disability. Today, there is no need to give up hope, because technology is an effective aid to rehabilitation. The difference is substantial between regaining self-care ability and relying on assistance for basic activities like eating or drinking.
So it is worth getting a device and (also) persevering with rehabilitation exercises at home.