Transcutaneous electrical nerve stimulation (TENS) is a method of electrostimulation that reduces or eliminates pain by activating your body’s natural pain relief mechanisms. The main targets of TENS are your nerve pathways that transmit pain stimuli and the system that produces your own pain-relieving substances. TENS treatment is symptomatic, i.e. it does not cure the underlying disease itself, despite eliminating the pain. Its main advantage is that it replaces medication (or at least the amount needed is less) and you can reduce unwanted side effects.
Efficacy of transcutaneous electrical nerve stimulation
The effectiveness of transcutaneous electrical stimulation may vary depending on the location and type of pain and the TENS program used.
All relevant research concludes that TENS provides significantly greater pain relief than placebo interventions. The results of the studies vary, which is also due to the fact that different stimulation pulses (different frequencies, amplitude, treatment duration) are used. All studies are consistent in considering transcutaneous electrical stimulation (TENS) as a suitable method for pain relief.
TENS refers to any electrical stimulation delivered through electrodes placed on the skin surface to stimulate sensory nerve endings and pain reduction mechanisms.
Mechanism of action of TENS
The tiny electrical impulse emitted by a TENS machine stimulates the sensory nerve endings in your skin, activating your natural pain relief mechanisms. It acts at two main points, the pain-transmitting nerve pathways and the endogenous opioid system. The parameters of the electrical stimulation determine which pain relief system is activated by the pulse.
Pain gate mechanism
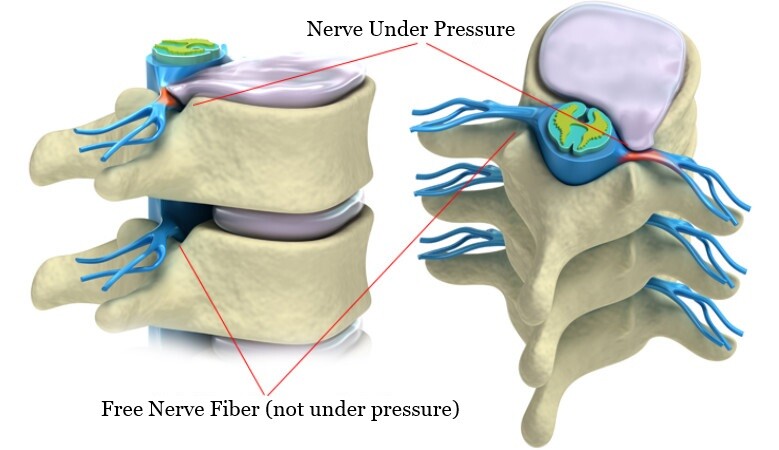
The pain gating mechanism is associated with the “Aβ” (A beta) sensory nerve fibres. Stimulation of these fibres reduces or eliminates the transmission of pain signals through the spinal cord to the pain centre in the brain. And if the pain signal is not transmitted, the pain sensation does not develop.
Empirical evidence indicates that the most effective stimulation for “Aβ” fibres is in the 90-120 Hz range, which is relatively high.
However, it’s important to note that there isn’t a single universal frequency that works for everyone. While frequencies within the mentioned range are often effective, the ideal frequency should be determined individually for each person.
For optimal pain relief, it’s advisable to acquire a device that permits treatment frequency adjustment to find the best frequency for you. While you can achieve pain relief with the default settings on TENS devices, these may not be the most effective treatment for your specific needs.
Endogenous opioid system
When used at slow frequencies of 2-5 Hz, these stimulate the “Aδ” (A-delta) fibres. Their activity stimulates opioid mechanisms and increases endogenous opiate (encephalin) production in the spinal cord. Encephalin has a strong analgesic effect and also reduces the activity of pain transduction pathways.
As with the way the pain gate works, there is no single, magical frequency that is equally effective for everyone. Everyone needs to find the frequency that works best for them.
TENS devices and their programmes
Simpler TENS units offer traditional TENS programs like high (conventional TENS) or low frequency (endorphin TENS), typically effective for short-term pain. However, these programs lead to habituation, with results diminishing after a few days. In contrast, quality devices provide programs like Burst, Modulated TENS, or Microcurrent (MENS) to avoid habituation, offering long-lasting effects as the brain can’t filter them out.
What can you do to avoid habituation?
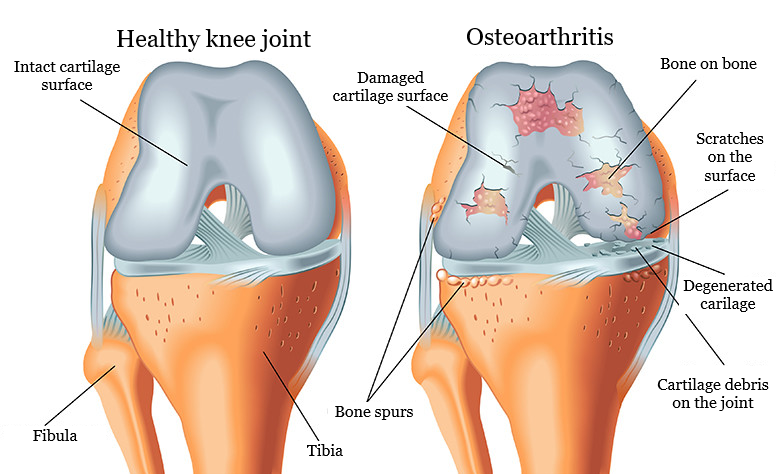
For short-term pain like toothaches, muscle strains, and sprains, you can use a cheap TENS unit. Since it’s most painful in the first few days natural healing reduces pain. But if you have chronic conditions like arthritis or herniated discs, opt for a TENS unit with modulated TENS or microcurrent therapy to prevent habituation and maintain effectiveness during long-term use. These modern devices may be more expensive, but they provide lasting relief for chronic pain.
Before choosing a TENS unit, think about how often you need to relieve your pain. If it’s usually 4-5 days, then cheap TENS may be good, but if it’s more than a week for a flare-up, then you need a device that provides modulated TENS or microcurrent (MENS) treatment.
Here you can read about how to use a quality TENS unit for ailments that you may have with success.
Side effects of TENS
Transcutaneous electrical stimulation clearly has fewer side effects than what one would expect with the long-term use of pain medications.
The most common complaint is reddening of the skin at the treatment site. However, this is usually only due to the local capillary dilating effect of the electrical pulses. It disappears 15-20 minutes after the treatment. If it does not disappear and the site swells, you may be allergic to the adhesive or gel of the self-adhesive electrode. Replace the electrode with a different type from another manufacturer and this usually helps.
I wrote about what conditions TENS should not be used for in this article.
Accurate information to know before TENS treatment
Never treat new pain with a transcutaneous electrical nerve stimulation (TENS) device if it occurs suddenly, consult a doctor first. In general, it is true that you should only treat pain for which you know the cause. If your doctor has recommended pain medication, you can choose TENS treatment instead of pain medication. Only a mentally competent patient should use a TENS unit independently.
If you have a pacemaker, transcutaneous electrical nerve stimulation treatment is generally not recommended. It is not ruled out but should be carefully and carefully assessed. You should not apply it near the pacemaker on the chest, back, shoulders or neck.
Placing electrodes in the chest, abdomen, and pelvic area during pregnancy is contraindicated. A recent study suggests that, although TENS is not the ideal (first-choice) treatment option during pregnancy.
TENS pain relief during work (for example, sitting in your office chair) is safe and effective. However, never use it while driving, operating heavy machinery or working at height!
If you are allergic to the electrode gel or adhesive, do not use it with a self-adhesive electrode. In this case, use a rubber (silicone) electrode. Avoid applying electrodes to areas with skin issues, the neck’s front, or near the eyes.
Typically, doctors do not advise using stimulation when treating patients with epilepsy, so consult your doctor.