Diabetes is one of the most common diseases today. The disease is “insidious”, as it causes no pain or complaints for a long time, meaning it can easily remain hidden. Complications are often the only discovery trigger. One of these is diabetic foot, which can slowly lead to a serious condition, even the dreaded amputation.
Diabetic foot lesions are most commonly caused by a triad of blood supply disturbance (ischaemia), neuropathy and infection. One of the dreaded complications of diabetes is amputation, the loss of a limb.
Statistics on complications of the diabetic foot: [1]
- Complicated leg fracture is responsible for a significant proportion of diabetic amputations.
- 20-40% of diabetes treatment costs are related to the management of the diabetic foot.
- 7-10% of people with both diabetes and neuropathy also develop ulcers.
- Amputation occurs within one year of ulceration in 5-8% of patients.
- A leg ulcer is present in 85% of diabetes-related amputations.
- Diabetes increases the risk of amputation eightfold in patients older than 45 years, 8 to 12 times in those older than 65 years, and 23 times in those between 65 and 74 years.
Diabetic neuropathy
Around 40% of people with diabetes have some degree of neuropathy. The consequences may include pain, sensory disturbance or movement disorders. One of the most important problems in the development of diabetic foot is the lack of sensation of the foot, the rubbing of the shoe, which can cause sensory disturbance. This leads to tissue damage, ulceration and deformation of the foot and encourages infections.
Diabetic ulcers and prolonged wound healing
- Peripheral arterial disease (PAD, also known as vasoconstriction) is thought to be the cause of the blood supply problem in diabetic feet.
- The risk of developing vascular stenosis is significantly increased by diabetes. Ischaemia is the main factor preventing wound healing.
- Diabetic neuropathy and blood supply disturbance together are known as neuro ischaemia. In these cases, wound healing is influenced by the severity of the blood supply disturbance.
Infections
- The most common sign of infection is an increase in wound exudate. [1]
- The infection makes it difficult to balance diabetes. [1]
- In the absence of treatment, infections on the diabetic foot can spread rapidly to other parts of the body and can even lead to life-threatening generalised septic infections [1]
Symptoms of diabetic foot

- Muscle weakness in the muscles of the foot, ankle, leg or hand
- Forceful posture and pain when walking
- High arch or very flat feet
- Numbness in the legs, arms and hands
Medical management of diabetic foot
- Prevention is more important, with a focus on keeping diabetes in balance and blood glucose levels within the normal range
- Treating established diabetic wounds by cleaning, disinfecting and dressing
- The use of antibiotics is recommended for all infected wounds in combination with wound management [1]
- Surgery is required if the infection has resulted in
- an abscess develops
- the infection extends to the bones or joints
- severe necrosis, gangrene or necrotizing fasciitis[1]
Physiotherapy treatment of diabetic foot
- The purpose of using physiotherapy methods is twofold.
- The aim is to prevent the development of complications.
- On the other hand, to alleviate the symptoms of the diabetic foot that have developed. [4]
- Physical therapists also play an important role in patient education
- teaching foot care and wound care
- teaching correct posture, gait and walking[4]
- instruction on the prevention of amputation
- A number of clinical studies have demonstrated the effectiveness of TENS treatment in reducing pain caused by diabetic neuropathy. [5]
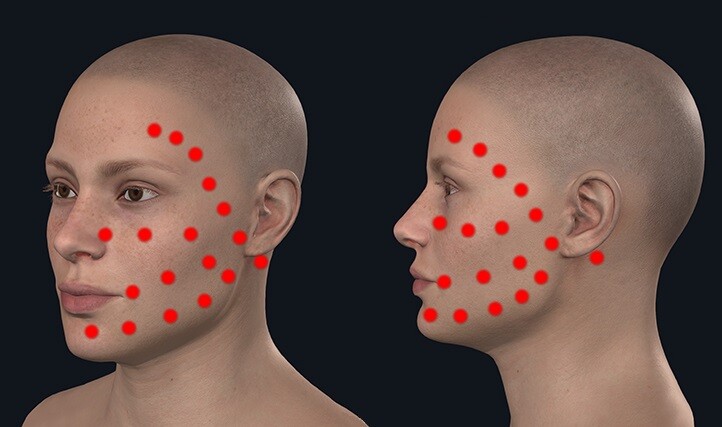
- Recent studies report the beneficial effects of soft laser treatment in both healing diabetic ulcers and relieving neuropathic symptoms.
I recommend B-Cure soft laser devices for the treatment of diabetic ulcers and neuropathy.
B-Cure Classic Soft Laser
Alternatively, there are higher power class soft laser devices. These soft lasers deliver 5 Joules more rapidly, shortening the treatment time to 10-12.5 seconds compared to 6 minutes per spot.
Personal Laser L400 soft laser
High-end soft laser
EnergyLaser L500 Pro Bluetooth Soft Laser
Sources
- Lepäntaloa M, Apelqvistc J, Setaccie C, Riccof JB, de Donatoe G, Beckerg F, Robert-Ebadig H, Caoh P, Ecksteini HH, De Rangok P, Diehml N. Chapter V: Diabetic Foot. European Journal of Vascular and Endovascular Surgery. 2011;42(S2):S60-74.
- Zakaria HM, Adel SM, Tantawy SA. The Role of Physical Therapy Intervention in the Management of Diabetic Neuropathic Foot Ulcers. Bull. Fac. Ph. Th. Cairo Univ. 2008 Jul;13(2).
- Youtube Video: the Diabetic Foot Exam https://youtu.be/aVz-Ja9Grvg.
- Kalra S, Kalra B, Kumar N. Prevention and management of diabetes: the role of the physiotherapist. Diabetes Voice. 2007;52 (3).
- Dubinsky RM, Miyasaki J. Assessment: Efficacy of transcutaneous electrical nerve stimulation in the treatment of pain in neurologic disorders (an evidence-based review) Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2010 Jan 12;74(2):173-6.
- Pedrosa HC, Leme LA, Novaes C, Saigg M, Sena F, Gomes EB, Coutinho A, Borges Carvalho WJ, Boulton A. The diabetic foot in South America: progress with the Brazilian Save the diabetic foot project. International Diabetes Monitor. 2004;16(4):17-23.
- Turan Y, Ertugrul BM, Lipsky BA, Bayraktar K. Does physical therapy and rehabilitation improve outcomes for diabetic foot ulcers?. world journal of experimental medicine. 2015 May 20;5(2):130.